Gait Retraining Enhances Athletes’ Technique (GREAT) Running
June 30, 2021 | Download PDF
Military service members continue to sustain traumatic anterior cruciate ligament (ACL) injuries at a high rate in training and sports-related activities. The significant lost duty time, poor self-reported functional outcomes, and long-term disability caused by these injuries directly leads to degraded operational readiness and exorbitant costs to both the Military Health System (MHS) and the Department of Veterans Affairs. After surgical reconstruction to repair the anterior cruciate ligament (ACLR), less than half of Service Members return to full duty. Knee strength and lower extremity biomechanical asymmetries during running are commonly observed in the civilian general population following surgery and have been shown to contribute to greater self-reported disability, greater risk of knee re-injury and the progression of knee osteoarthritis. However, the presence of asymmetries in military Service Members following surgery and how they relate to symptoms, function and further joint degeneration throughout recovery are not well known.
In 2018, researchers of the Keller Army Community Hospital (KACH), Baylor University – KACH Division I Sports Physical Therapy Fellowship at West Point, New York embarked on a project titled, “Gait Retraining Enhances Athletes’ Technique: (GREAT) Running,” to explore whether some of the key factors that affect civilians’ rehabilitation and functional outcomes following ACLR also affect our Service Members. In addition, the team sought to assess a wireless wearable in-shoe biofeedback sensor (Loadsol®) to detect landing biomechanics in Service Members and assess the relationships among the landing patterns and hop performance, levels of biomarkers representative of chondral injury, patient reported outcome measures, running biomechanics, and knee strength following ACLR. The final deliverables of the project will speak to the ‘Quality, Readiness and Reduced Cost’ pillars of the Advanced Medical Technology Initiative (AMTI) Program.
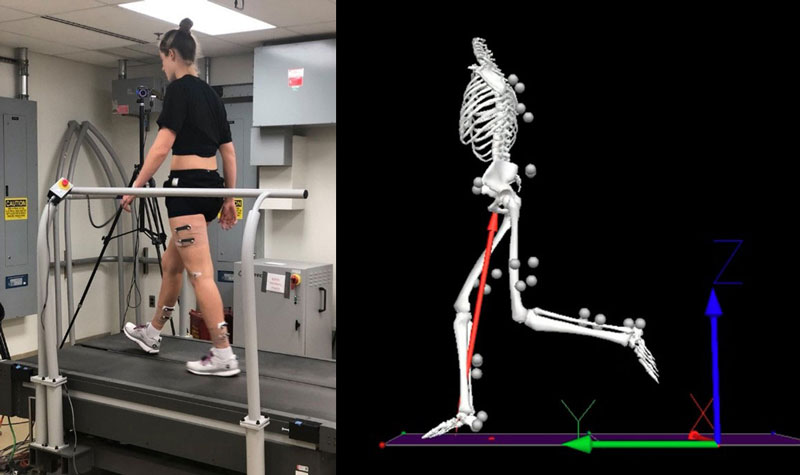
So far, the team has observed significant lower extremity asymmetries in measures of knee strength (quadriceps peak torque) and running biomechanics (peak knee flexion angle, knee flexion angle at initial contact, heel-to-center of mass distance at initial contact, peak internal knee extensor moment, peak vertical ground reaction force and braking impulse) when Service Members were cleared to return to running activities (approximately 5 months post-surgery). The team’s novel preliminary results suggest that there is a large-magnitude of unresolved knee strength deficit and lower extremity running biomechanical asymmetries post-ACLR in military Service Members. This is concerning, considering reduced strength, and asymmetrical movement patterns following ACLR may contribute to development of knee osteoarthritis and increased risk for re-injury. From a clinical perspective, these data indicate that military Service Members are being cleared to return to run when their surgical limb physical impairments indicate that they may not be strong enough or move safe enough to do so. Military clinicians may need additional guidelines focused on restoring quadriceps strength limb symmetry before initiating return to running to mitigate potentially harmful running biomechanics asymmetry and subsequent knee damage in Service Members after ACLR.
The preliminary results of this AMTI project were accepted for platform presentations at both the 2021 American Physical Therapy Association Combined Sections Meeting and the 2020 Military Health System Research Symposium (MHSRS). Additionally, the project was one of 12 out of 258 abstracts accepted for an oral presentation in the Young Investigator Breakout Session, and subsequently on the short list for the MHSRS 2020 Young Investigator’s Award.
Results from additional project deliverables, to include the efficacy of the Loadsol® are forthcoming. The Loadsol® is an in-shoe insole system that enables measurement of force between the foot and the shoe during dynamic movements. Traditionally, force has needed to be measured in a research laboratory, however, Loadsol® technology offers military clinicians the ability to measure important movement biomechanics right in any MHS physical therapy clinic. The system is user friendly and has options to provide real-time auditory, visual or vibratory feedback to patients on relevant biomechanical parameters such as peak force, step rate, average vertical loading rate, contact time and symmetry.
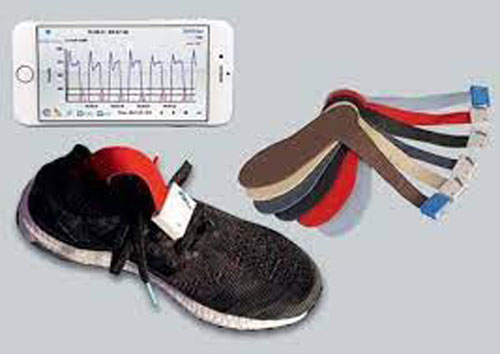
Information from the preliminary analysis of Loadsol® will be used to plan future efforts assessing the wearable insole technology’s usefulness to assess symmetry of movement patterns in Service Members after ACLR. The team is also currently processing results to better understand the relationships among levels of biomarkers representative of chondral injury (osteoarthritis markers) with patient reported outcome measures, running biomechanics, and knee strength following ACLR. Results from the remaining deliverables will be submitted for presentation at the MHSRS Conference in 2022 and submitted for peer-reviewed publication.
Despite pandemic-related delays and roadblocks, this novel AMTI demonstration project represents the first to provide insight into military Service Members’ knee strength and running biomechanics after ACL injury. The knowledge that strength and movement deficits not only exist, but that some exist at a greater magnitude in our Service Members than in civilians following surgery, and what other clinical factors they are related to, is important. This information can help military clinicians re-assess their clinical outcomes and benchmarks and enhance therapeutic interventions. In civilian populations, these movement patterns and strength deficits do not resolve long term and may contribute to return to duty limitations in Service Members. Since both knee strength and running biomechanics are modifiable factors, the team’s future work will seek to examine the effect of strength and gait retraining interventions using the Loadsol® technology to improve these important outcomes in a military population.
The significance of this project on the MHS is indisputable. Effective evidence-based and clinically feasible rehabilitation screening and intervention tools targeting post-injury physical outcomes are essential for reducing the adverse impacts of ACL injuries to both the individual Warfighter and the MHS. The preliminary results of this project represent the first step towards identifying knee strength and running biomechanical factors of which we can focus therapeutic interventions to improve return to preinjury levels of activity in this population, as well as long term joint health. This data is essential to improving our military’s lives and welfare, who sustain an ACL injury and undergo ACLR while in service to their country.
The Lead Project Innovator, MAJ Bryan Pickens, summed up this effort stating, “This project and the knowledge we have obtained is critical in advancing the post-operative management of individuals with ACL injury. Targeting the asymmetries observed in this study may serve to improve return to duty rates and mission readiness in military service members. This critically important work would not be possible without the support of TATRC’s AMTI Program. The AMTI Program has been pivotal in the execution of this novel demonstration project. Without AMTI’s funding, strategic mentorship and unwavering support the project would not have been possible. With AMTI’s continued guidance we hope to expand the results of this project to improve the clinical resources available to military providers for improved decision making and in-clinic detection of potentially injurious strength and movement asymmetries following ACLR that may contribute to poor full return to duty rates.”
For additional information on this AMTI funded project, please contact Ms. Holly Pavliscsak at holly.h.pavliscsak.ctr@mail.mil.
This article was published in the January 2022 issue of the TATRC Times.