Working Towards Interoperable Medical Device Systems, a Key Component of Military Medical Modernization
Tuesday, April 30, 2024 | Download PDF
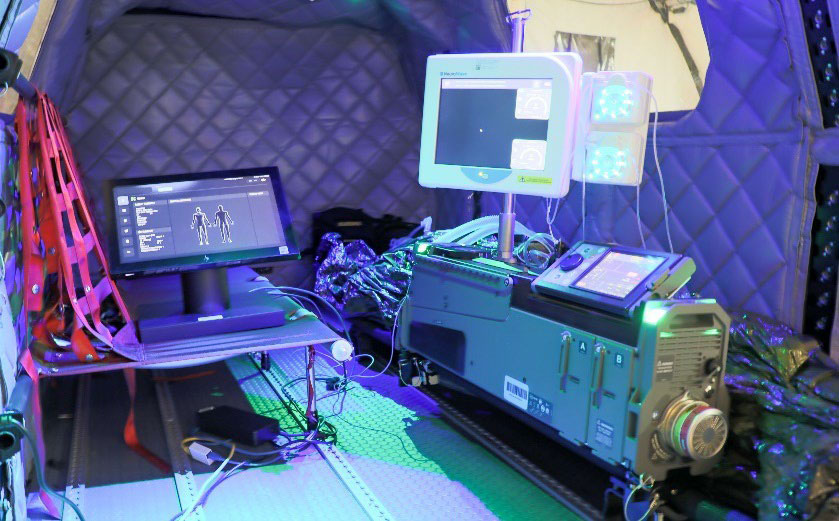 Figure 1: Proof of Concept Remote Patient Management System (RPMS). The RPMS is a medical device platform composed of mechanical ventilator, infusion pump, and patient vitals monitor devices designed to augment casualty care capability and capacity during evacuation and pre-hospital environments.
Figure 1: Proof of Concept Remote Patient Management System (RPMS). The RPMS is a medical device platform composed of mechanical ventilator, infusion pump, and patient vitals monitor devices designed to augment casualty care capability and capacity during evacuation and pre-hospital environments.
The complex intelligent systems that create the interconnected digital world of today rely on effective data integration. Quick and reliable transmission and storage of data between devices is just one part of this equation. The shared data must also be written and stored in a standard data format such that it is understandable across a system. Imagine attempting to read a book written in a different language. The original writer may have written an amazing piece of literature (such as the TATRC Times FY24Q2 Newsletter!), but to you, it just appears to be nonsense. Although the same information has technically been shared and recorded, its utility is greatly diminished when other devices cannot comprehend the shared data. Est-ce que tu comprehends? Capisci?
 Figure 2: Automating the DD 1380, or Tactical Combat Casualty Care Card, allows the combat medic to have greater capability and capacity to deliver care by giving the medic time for more physical tasks by reducing their task burden.
Figure 2: Automating the DD 1380, or Tactical Combat Casualty Care Card, allows the combat medic to have greater capability and capacity to deliver care by giving the medic time for more physical tasks by reducing their task burden.In much the same way, medical data can suffer from similar limitations. Currently, medical devices from different manufacturers often store patient medical data in different formats. For patient data recorded from one device to be used by another device in the system, it must then be translated into a common data format. A critical aspect of medical data interoperability that is often overlooked is Where and When the data is translated into a common language (data model), which can have a large impact on the functionality of the overall system. In TATRC’s Remote Patient Management System (RPMS) (see Figure 1) and Automating Casualty Documentation Projects (see Figure 2), prototype concept systems are being developed that translate medical data from various devices into a common data standard in real time at the point of care.
Figure 3 compares two data integration approaches in which medical data from multiple devices is collected from a battlefield care encounter and then transmitted into the cloud to be accessed at a remote site. In the current process (left), medical data is typically integrated together only after patient care has ended and the recorded medical data is being entered into an EHR. However, in the RPMS approach (right), data is integrated locally and in real time into a single shared data set.
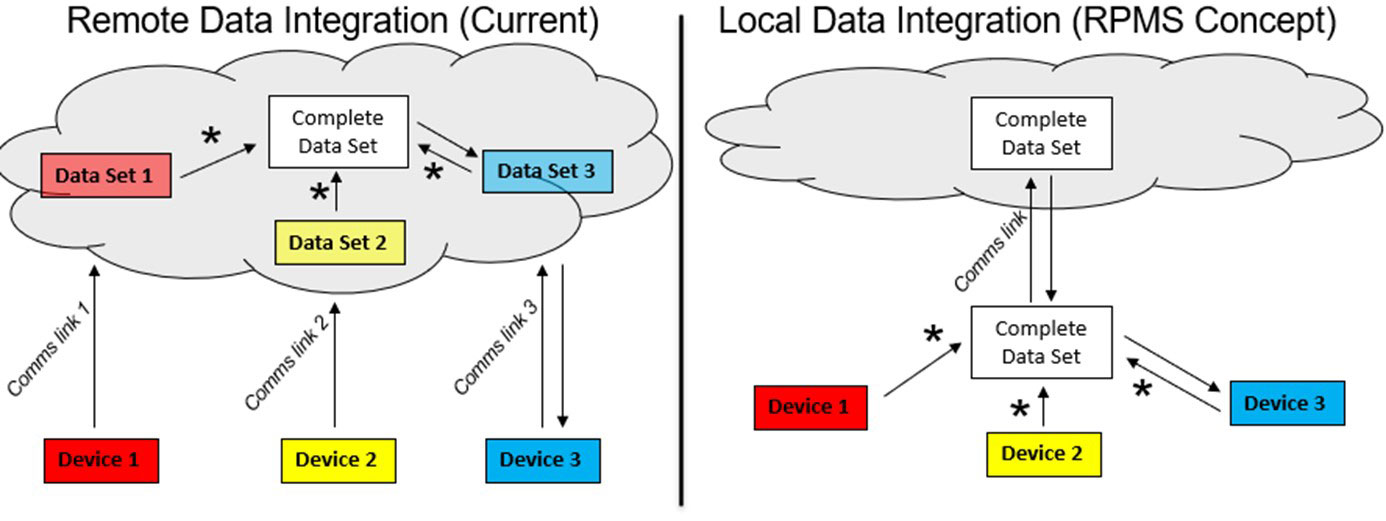 Figure 3: This figure compares two data integration approaches in which medical data from multiple devices is collected from a battlefield care encounter and then transmitted into the cloud to be accessed at a remote site.
Figure 3: This figure compares two data integration approaches in which medical data from multiple devices is collected from a battlefield care encounter and then transmitted into the cloud to be accessed at a remote site.
This updated approach has a variety of system-level benefits for patient care. For example, it can streamline telemedicine and allow a remote care provider to better support local care. In the system on the left, the data transmitted from each separate device would have to be remotely viewed on a separate software package, webpage, or physical device entirely. With the novel approach on the right, the remote care provider can view all patient data and control device settings with the same standard user interface. With better visualization of all patient information, a remote expert is empowered to provide effective and timely care in time critical and medically complex care situations. In addition, they can more simply view patient data and provide care assistance to multiple patients in various locations.
The RPMS approach for telemedicine can also allow for more efficient use of bandwidth over tactical networks. A locally integrated data set can be transmitted from a single communications link and can be optimized to send patient data based on situational need. For example, a remote expert may require real-time access to bandwidth-heavy data to care for a critical patient. However, they may only require low-bandwidth transmission of essential vitals signs for basic monitoring for a stable patient, thus freeing up bandwidth for other operational uses. Finally, the local data integration approach enables the introduction of autonomous control of medical care, in which AI or a closed loop control algorithms can use patient data from multiple devices to manage resuscitation or provide intelligent alerts to providers. TATRC is exploring the variety of potential benefits for this care model in which patient management tasks are shared between local providers, remote experts, and intelligent algorithms operating at the edge. A common data model must be introduced at the point of care to realize these potential benefits, and is a key enabler to TATRC’s Autonomous Casualty Care portfolio in our aim to modernize military medicine to meet the demands imposed by our future operating concepts.
For more information on this initiative, contact Mr. Nate Fisher at nathan.t.fisher3.civ@health.mil.
This article was published in the April 2024 issue of the TATRC Times.