2B-Healthy: BHSAI’s AI System for Early Warning of Adverse Conditions in Humans
March 31, 2021 | Download PDF
Because early detection of exposure to pathogens from biological weapons or emerging infectious diseases is critical for maintaining Force Health Protection, Dr. Jaques Reifman, Director, of the Biotechnology High Performance Computing Software Applications Institute (BHSAI) here at TATRC, led a team to develop the 2B-Healthy app for automated, real-time detection of abnormal vital signs. Consisting of commercial-off-the-shelf (COTS) hardware and customized software, the 2B-Healthy app pairs a non-invasive wearable device that continuously collects vital-sign data with a proprietary algorithm that identifies physiological changes associated with abnormal events, including infection. To this end, this exciting new Army technology serves as a self-sufficient, early-warning, bio-threat detection system that allows for rapid situational awareness and time-sensitive deployment of countermeasures, such as evacuation, quarantine, and treatment of infected Service Members.
2B-Healthy was a collaborative effort between the U.S. Army, CPT Sidhartha Chaudhury who now serves at the Walter Reed Army Institute of Research, staff at BHSAI, and the U.S. Naval Medical Research Center (NMRC). The 2B-Healthy project was sponsored by the U.S. Defense Threat Reduction Agency.
Elements of traditional physiological modeling combined with hardware suitable for field environments allowed for real-time monitoring of subjects under every-day ambulatory conditions. With the use of non-invasive wearable devices and mobile computing technologies to collect and analyze continuous vital-sign data from subjects in controlled human infection studies, the research team used computational methods, including a machine-learning algorithm, to detect vital-sign deviations indicative of infection. This enabled the development of a model for predicting the likelihood of infection directly from continuous vital-sign data, and its implementation as an app capable of real-time infection detection.
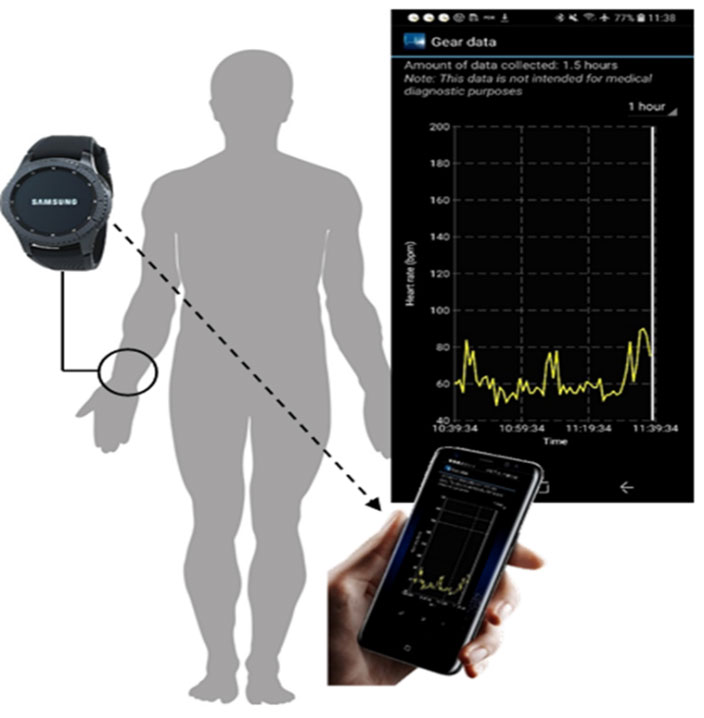
This project piggybacked on a controlled human malaria infection (CHMI) study performed at the NMRC. A malaria infection challenge was chosen because it is an established clinical model with a well-defined time course and symptoms of infection, has direct clinical and military relevance, a known time of exposure and infection, a long incubation period that allows time to make predictions, and early- and late-stage diagnostic tests approved by the FDA. The study used wearable technology in the form of a Samsung Gear S3 smartwatch to collect continuous vital-sign data from volunteers, and then wirelessly transmitted it to a Samsung Galaxy S8 smartphone where the machine-learning algorithm resides (see Figure 1).
Subjects in the CHMI study received wearable devices and collected vital-sign data for at least 12 hours per day, with the first 2 weeks collected during normal activity. Subjects were then deliberately exposed to malaria-carrying mosquitos in a controlled setting (Day 0) and resumed their daily activities (for example, lived at home, went to work, exercised) while being regularly monitored for symptoms by clinical investigators. On Day 9 after the malaria challenge, the subjects checked into a hotel at night for daily monitoring by the clinical team, including blood-smear tests, the clinical gold standard diagnostic for detection of blood-stage parasitemia. At the first sign of infection, subjects received an FDA-approved antimalarial drug to clear the infection.
In the CHMI study, heart rate, skin temperature, and 3-axis accelerometer data were collected from subjects for 6 weeks. The vital-sign data collected 2 weeks before infection defined an individualized baseline for each subject so that predictions of infection could be made. Subjects were challenged with malaria at the end of week 2, and monitoring continued for 4 additional weeks so that data could be collected during the incubation (pre-symptomatic) and symptomatic infection periods. In addition to the CHMI study, a second baseline-data collection study was conducted and used as a control for developing the algorithm. The same vital signs of heart rate, skin temperature, and activity data were continuously monitored using the smartwatch/smartphone hardware for 4 weeks in healthy, non-infected adult volunteers.
With the use of the vital-sign data from both studies, the 2B-Healthy infection-prediction algorithm was developed. It consists of two steps: 1) detection of abnormal heart rate patterns while accounting for circadian rhythm and physical activity and 2) estimation of the probability of infection using a model that accumulated evidence of abnormal heart rates over time. In over two-thirds of the CHMI subjects, the model correctly predicted infection and allowed for early detection, on average 6 days before parasitemia (a very early test of infection). The study results correspond to an overall sensitivity of 78% for infection detection and 67% sensitivity for early infection detection (before parasitemia), validating the algorithm as a screening tool. Dr. Reifman noted that “control studies, such as the CHMI, are the perfect mechanism to assess the potential benefits of wearables and the Army’s infection-detection algorithm, because in this type of study we know exactly when the infection occurred and have very sensitive assays to detect infection as early as possible. These allowed us to obtain a very accurate assessment of the algorithm’s performance, which is supported by accurate and timely clinical data.”
The U.S. Army Medical Research and Development Command has filed multiple U.S. and international patent applications for the 2B-Healthy system.
The successful development of the 2B-Healthy app provides the U.S. military with the capability to carry out automated, rapid detection of Service Member infection, including SARS-CoV-2-infected individuals, before they are able to infect others around them. This will be essential to restoring and maintaining Force Readiness during the current COVID-19 pandemic as well as future ones. As Dr. Reifman stated, “we now know that by integrating COTS wearables, as imperfect as they may be, with customized AI algorithms tuned to an individual, we are able to provide early indication of an abnormal event, including human infection.”
For more information on this project, please contact Dr. Jaques Reifman, jaques.reifman.civ@mail.mil.
This article was published in the July 2021 issue of the TATRC Times.