NETCCN Overview
The National Emergency Tele-Critical Care Network project (or NETCCN – rhymes with “Jetson”) addresses a critical problem for COVID response: Where there are no ICU beds, there are no critical care trained clinicians. And even where there are ICUs, especially during surge situations, there are not enough of the right kinds of trained clinicians. NETCCN is an evolving network of clinical care teams that provide expert medical advice, particularly related to the management of critical illness from severe COVID-19 infection, to any individual who needs it using mobile device applications. The simple act of supporting local caregivers from family member to nurse to general practitioner to surgeon – anyone without critical care knowledge, skills, or abilities – with expertise from remote tele-critical care specialists enables these caregivers to provide more support to patients than would otherwise be possible.
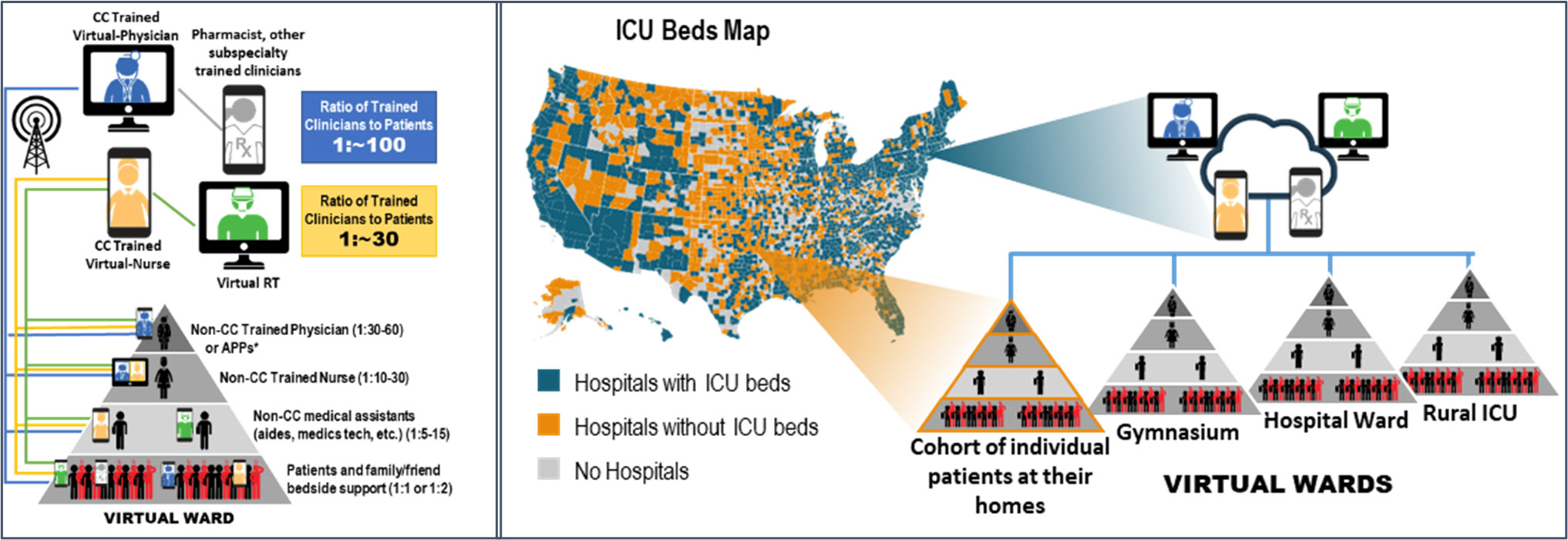
Fundamentally, NETCCN is designed to be rapidly deployed, easy to use, and intended to help with tiered staffing models[1] where local, non-critical care trained clinicians can have a critical care trained expert in the palm of their hand (figure). Other examples of how NETCCN clinicians have helped hospitals and local care teams:
- Back-up support for fixed Tele-Services. For example, when a fixed camera was frozen and the bedside team could not quickly reset the system, they instead engaged a remote NETCCN provider using an iPad and the NETCCN application to get eyes on the patient, immediately helping the local team to assess and manage a patient who was rapidly desaturating and struggling to breathe.
- Relieving anxiety. There is a high level of fear and anxiety when caregivers, inexperienced or forced by necessity, manage patients outside or at the limits of their scope of practice. Small, rural hospitals in the midst of a surge – or even tertiary care medical center that are over-run by patients as was the case in New York City - must often manage patients who are critically ill for longer than normal because referral hospitals are full. When patients meet the local care standard for transferring a patient to the next “level” of care, but are unable to do so, NETCCN remote experts are there to help. They can patiently guide the local care teams to best manage patients while awaiting transfer using whatever resources are available locally. In some cases, this type of support can relieve transfer burden on the referral hospital by giving local care teams the confidence needed to continue managing a patient without transfer.
- Relieving task saturation. Local care teams get busy, especially during a surge. Documentation of patient care and keeping track of orders can be a daunting task. Even without EMR connectivity, remote NETCCN providers can help local care teams with documentation and orders in the NETCCN application, which can then be sent to the local hospital electronically or by Fax for printing into a hard chart or uploading into the local EMR.
- Relief. Local critical care experts – nurses, doctors, RTs – may be called upon to be continuously available to “supervise” their local team who is not familiar with critical care tasks like managing continuous sedation or trouble shooting a ventilator or managing multiple organ failure. These precious resources make work days work weeks at a time with minimal sleep and no time off. NETCCN can help by providing any amount of coverage for local teams – a night, a day, a weekend. Whatever is needed to allow local critical care experts to recharge and get back into the fight.
- A second set of eyes. When task saturated and/or burnt out, a second set of eyes helping local care teams identify missteps or care lapses or missed opportunities can significantly improve the quality of care. NETCCN experts never patronize local caregivers, but are available to talk through complex cases and help local teams make good catches.
- A second set of “brains.” Local care teams can be overwhelmed during a disaster and may not be available at all times. When a care team is managing one emergency, another emergency may occur at different location. While waiting for the local experts to become available, NETCCN remote experts can help local caregivers make diagnostic decisions by ordering appropriate tests so that necessary information is made available for the local experts to act upon as soon as possible. In some, life-threating situations when local expertise is not available, NETCCN remote experts can even coach local caregiver through advanced procedures like needle or tube thoracostomy to relieve tension pneumothorax.
- Remote Home Monitoring and Hospital at Home Services. Monitoring patients at home, whether before they present to a hospital for services or after discharge, can help improve hospital capacity by ensuring only patients who need hospital services are admitted and by keeping others at home. NETCCN, while monitoring patients at home, has helped identify those who would benefit from oxygen and has sent it to the patient’s home – without a hospital visit! Similarly, patients recovering from severe illness may be able to go home earlier with appropriate oxygen support and routine telemedicine monitoring using a NETCCN application. Overall, home monitoring and home based “hospital like” care support optimizes hospital resources and maximizes hospital bed capacity. In some situation, the local EMS or other home medical service providers can help provide additional resource like IV placement or wound care. Home monitoring also helps to relieve patient anxiety by providing them reassurance that someone is monitoring their symptoms and can be available on demand if needed.
- Palliative care. Despite our best efforts in medicine, sometimes patients die. Our teams have helped facilitate end-of life care for patients in the hospital, and at home using NETCCN applications on patients’ personal cellphones. We can connect a patient with social workers and other experts to help address all manner of concerns including pain control, spiritual health and emotional support.
- Opportunity. Unfortunately, healthcare workers get sick also. If a local critical care expert gets sick, they can help their team by becoming a NETCCN remote expert! Because the NETCCN provider applications are web-based, they can be accessed from anywhere. On-boarding as a remote expert is simple and clinicians in quarantine or isolation can become NETCCN remote experts in less than 48 hours.
An alternative use case for the NETCCN is for local hospitals/healthcare systems to “license” the application (i.e. get permissions to use one or more of the NETCCN platforms) to deliver services within their own hospital/healthcare system using their own clinical staff.
The NETCCN solutions are downloadable, HIPAA compliant, cyber secure applications on an iOS or Android phone or tablet that facilitate point of need teleconsultation with a remote critical care expert (physician, nurse, or respiratory therapist). Once the application is downloaded, it is simple for a patient or a local care team member to register himself/herself or a patient/family member. Training to use the application is minimal if needed at all.
Secondary functions of the NETCCN applications:
- Cohort patients in “virtual wards” and can assign local and/or remote care teams to these patients for consultation with the patient/patient designee or between care team members
- Facilitate simple documentation of patient demographics and important information for sharing across the care team
- Facilitate simple documentation of care team communications for the purpose of documenting recommendations and orders
- Allow documentation (notes, orders, etc.) to be transferred to local EMRs either by PDF or, in some cases, electronically
Future functions of the NETCCN applications:
- Remote monitoring of patients using some wearables and/or some medical monitors
- Full EMR integration with major EMR vendors
- Remote control of some IV pumps and mechanical ventilators
What NETCCN support requires?
- Waiver of state licensure requirements (i.e. cross state licensure for telemedicine) by law or executive order
- A local clinical, IT, and administrative champion willing and available to help solve problems together with the NETCCN partner. These individuals must complete demographic survey information for the hospital and be able to define/negotiate requested services
- Rapid disaster privileging for NETCCN remote experts (doctors, nurses, respiratory therapists, as needed)
- Availability of personal or facility purchased mobile devices (cell phones or tablets); in some cases, a web interface can be used on a laptop or desktop computer
What NETCCN does not need?
- Access to the local hospital network
- Installation of any hardware or wiring
- Insurance coverage
- Payment for disaster services (sustainment of service beyond government dictated time periods is not permitted unless it is purchased by the local hospital)
Reference:
1. https://www.sccm.org/Blog/March-2020/United-States-Resource-Availability-for-COVID-19